Cardiac surgery: a patient from Montpellier University Hospital celebrates ten years under assistance


Professor Gaudard, here with the complete Heartmate 2™ device. Midi Libre – co-owner


The turbine of the device which allows blood to be sent to the aorta and supports the heart which is not contracting sufficiently. Midi Libre – co-owner
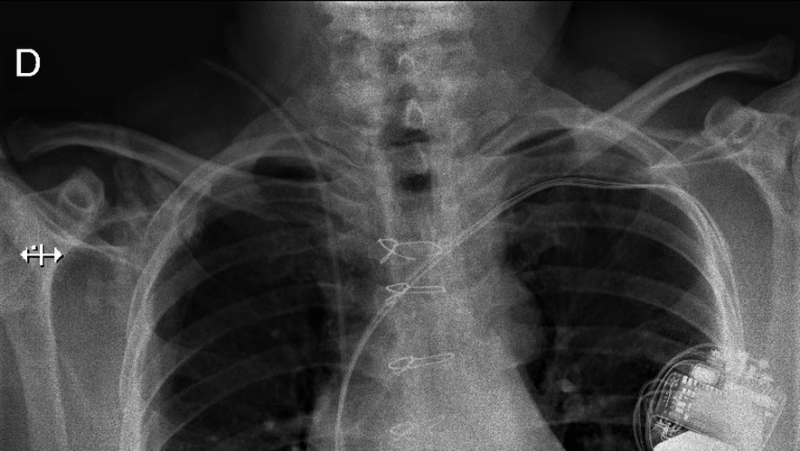
Le dispositif implanté dans la cage thoracique du patient. CHU de Montpellier
Appareillé en 2013, il vient de franchir un cap symbolique. Une nouvelle preuve de la maturité du dispositif dont le centre hospitalier montpelliérain est l’une des références.
"It’is a little restrictive but we are on earth!", cowardly, all in all, Pascal Dubuc. A long-time patient at the Montpellier University Hospital, he celebrated his ten years under the close control of Heartmate & trade just before the holidays. Or a cardiac assistance device of which the Arnaud-de-Villeneuve establishment is one of the French references in the matter.
"When I was implanted, I was in a coma. I woke up to a beautiful game console! It was a surprise. It's a little scary and then you get used to it…. And as there was no other solution…", says cheekily, the one who is now a pioneer in the cardiac surgery department.
From Jarvik 7 to the heart of Carmat, forty years of innovation
On December 2, 1982, the world shifted a little further towards science fiction. When a surgical team from Utah implants Jarvik 7, a then revolutionary artificial heart, into the ribcage of a former dentist. Which will allow its host to live one hundred and twelve days almost independently. A few months later, a second patient will be implanted and will survive 620 days.
Closer to us, the French company Carmat is developing a completely artificial heart implanted in a 76-year-old patient at the Georges-Pompidou European Hospital, in 2013.
After encountering some difficulties, Carmat put the transplants on hold. Newly authorized, these are currently being carried out in parallel with a clinical study required by the High Authority for Health. A protocol in which the University Hospital participates, which will communicate on this subject at the appropriate time. One thing is certain: the Montpellier site (in the top five in France for heart transplants) is one of the eight designated across the territory to participate.
In the case of cardiac assistance, studies are still continuing to try to minimize the discomfort of the patient wearing said device. This is particularly the case when it comes to autonomy. Today, the batteries (and backup batteries) given to the patient allow him to last four days (at full charge).
There is also talk of replacing the charging process with the induction technique. But this comes up against problems of skin burns. The other area of work focuses on reducing infections linked to the orifice through which the percutaneous line connecting the device to the outside passes.
"In everyday life, there are little things
which you should pay attention to"
Because he has been living with this device for a decade, grafted into the rib cage and connected to batteries and a control panel via a percutaneous line (a sort of electrical cable, Editor's note) connecting the whole. Or a longevity considered "exceptional" by the healthcare teams. Usually, this device is supposed to compensate for the wait for a heart transplant and, in fact, implanted for a longer period of time.
Pascal Dubuc chose to live ten years in a row with this system attached to his body. Despite everything, having to deal with certain constraints. "On a daily basis, there are little things you need to pay attention to,” he concedes. Like the cable, don't hang it on a door handle. Or give up on sea bathing and fishing. so as not to end up like Claude François!", he says jokingly.
The shortness of breath of cardiac assistance in France
Worthily celebrated in the department at the end of the year, the ten years of cardiac assistance followed for ten years by the University Hospital is a success but also the tree that hides the forest. Proof, supporting figures: "A hundred people are established in France each year. This is not huge when we would expect three to four hundred. We are quite behind in Europe even if, after all, not everyone can qualify for respiratory assistance. Despite everything, those with insufficient health status have too limited access to it because it is a little-known technology, including among community cardiologists,” notes Professor Gaudard.
In his specific case, Pascal Dubuc benefited from the second iteration of the Heartmate ™ system. Currently, practitioners are using the third version of this system designed by the American company. The Illinois company was the first to build a special laboratory for radiopharmaceuticals, in the mid-1940s. It was again the company, in 1985, which launched the first HIV screening test (1985).
"We are around thirty
of patients under assistance"
A precarious comfort that he would soon have to leave, "the next operation, it will be the transplant!", he announces at 59 years old, afterward ;finally surrendering to the arguments of his doctors.
"We told him it’s now or never! While there is always an additional risk in reoperating on a heart, it arrives in better shape. Usually, the time frame for a transplant is between two and three years. There he was registered. Afterwards, by chance, it can be done within the year. Otherwise, within two years (*),” explains Professor Philippe Gaudard, head of the anesthesia-resuscitation department and deputy head of the heart, lungs and vessels division. Head of clinic in 2022, remaining loyal to the establishment, Professor Gaudard has been working for a long time to develop respiratory assistance techniques.
And the practitioner details: "At the University Hospital, we have around thirty patients under assistance, including seven to eight waiting for a transplant". Added to this are around twenty others who are not on cardiac assistance. Knowing that, year after year, the establishment carries out around twenty transplants. "It’is average (national, Editor’s note)", he continues.
But also that the implementation of this assistance is the aggregation of several quite complex processes. "Since 2008, we have had one hundred and ten establishments. But not all university hospitals have this authorization like, for example, in Nice or Nîmes. Only twenty have it,” continues Philippe Gaudard.
Especially since this surgical procedure requires four hours of intervention. Then "a week in intensive care accompanied by education of the patient before releasing him after three or four weeks with the taking of anticoagulants. It's a bit like a transplant, summarizes the doctor.
There, "it’is a partial heart which assists the left ventricle, most often affected, particularly in cases of infarction. A turbine pumps the blood and, with a cannula, reinjects it into the aorta to help the heart which is not contracting sufficiently, he characterizes. High-end mechanics.
(*) Pascal Dubuc is the second patient living for the longest time with this cardiac assistance in France. Some American patients have lived beyond the decade.
I subscribe to read more




